What is binge eating disorder?
Binge eating disorder is mainly characterised by episodes of recurrent binge eating behaviors. This disorder is understood as the behaviour of eating large amounts of food quickly, in a short space of time, in the absence of any hunger signal. Moreover, the person that suffers from this disorder, perceives that he/she is unable to control it; he/she feels unable to stop doing it and often experiences discomfort, deep feelings of both guilt and shame afterwards.
In this case, the act of eating does not respond to a physiological hunger signal but it is used as a strategy to cope with anxiety or discomfort.
There is a preference for both high-calorie and unhealthy foods such as processed foods (industrial pastries, fried foods, etc.). However, in some cases, episodes of binge eating can even occur with healthy food. For this reason, rather than focusing on the type of food, we should focus on the relationship that the person keeps with food and it should be assessed whether they use it as a strategy to reduce their discomfort rather than to satisfy their physiological hunger.
On the other hand, considering the feeling of loss of control, only signs such as stomach pain, episodes of indigestion or nausea as a result of the large amount of food ingested can stop or prevent this behaviour to happen.
Since people that suffer from binge eating disorder often hide their behaviour due to embarrassment, it is sometimes difficult to detect as it can apparently affect healthy people.
In this scenario, it turns out to be essential to clarify that binge eating disorder is not directly associated with people who are overweight or obese, although these metabolic diseases may be developed as a result.
Binge eating disorder was early recognised as such in 2014, with the latest update of the Diagnostic and Statistical Manual of Mental Disorders (DSM5). Indeed, this diagnosis has been ignored and invisibilised for many years.
Symptoms and causes
The main symptom of binge eating disorder is, as it has been already mentioned, the compulsive ingestion of a large amount of food in a short space of time. This means a higher intake than would normally be eaten by another person under the same circumstances, with the same nutritional requirements.
In addition, there is a feeling of lack of control over what is being eaten; either an inability to stop the eating behaviour or great difficulty in controlling what and/or how much is eaten, as well as guilt and/or shame about the binge eating.
According to the DSM-5, binge eating episodes are related to 3 (or more) of the following events:
1. Eating more quickly than usually
2. •Eating until feeling unpleasantly full
3. Eating large amounts of food without feeling hungry
4. Eating alone due to embarrassment about the amount of food eating
5. Feeling unhappy, depressed, guilty or ashamed afterwards
We have all eaten much more than we actually need to at special occasions (such as Christmas dinner). That’s why, it can be difficult to distinguish occasional overeating from binge eating disorder. In fact, for a diagnosis of binge eating disorder to be made, these compulsive overeating episodes occur, on average, at least once a week within a three months period.
In general terms, some warning signs that should be taken into account are the following:
- Eating when you are not hungry, to the point of feeling uncomfortably full
- Eating too fast, uncontrollably and doing it alone or keeping it in secret.
- Feeling in low mood, guilty, ashamed or upset after eating more than usual
- Avoiding social situations, especially those involving eating events
- Experiencing fear of disapproval from others
- Showing concerns about weight gain after binge eating or experiencing weight fluctuations
- Frequent and unsuccessful dieting
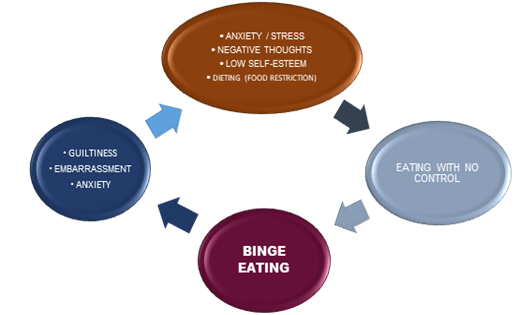
- Feeling desperate to break the binge eating cycle (see underlying image)
- Having low self-esteem related to your physical appearance
- Having anxiety and/or depression
To date, no specific cause of binge eating disorder has been identified since it is considered a multifactorial pathology.
On one hand, there seems to be a genetic predisposition although the associated underlying genes have not been identified yet. In fact, family patterns have been observed that seem to respond to neurobiological alterations. However, we cannot underestimate the weight of learning, as we tend to reproduce our family’s relationship with food.
Within the social level, we must take into account the significant pressure exerted, especially in powerful social networks, on the “perfect” physical appearance, the excessive concerns about healthy food intake and the concept of dieting itself. In order to better understand and explore this issue in depth, it may be helpful to read other sections in our blog about fatphobia and diet culture.
Within the psychological level, the lack of emotional management skills and therefore, of coping strategies in stressful situations or to manage negative feelings (failure, anger, boredom…) together with the presence of low self-esteem, anxiety or depression, contribute significantly to the development of binge eating disorder.
Risk factors
Both the causes and risk factors of binge eating disorder are closely related. The following can be identified:
- Age: Binge eating disorder can manifest itself at any age. However, adolescence is a particularly sensitive stage, when the first signs of binge eating disorder can be observed, especially towards the end of adolescence.
- Family history: the presence of eating disorders within our family determines the relationship we stablish with food.
- Personal history:
- Other disorders: having other eating disorders, anxiety, depression….
- Low self-esteem
- Having suffered some kind of abuse in childhood
- Poor coping resources to manage negative emotions
- Excessive concerns about body image and repeated exposure in the past to negative comments about their physical appearance / weight
- Low tolerance for failure
- Personality traits: being overly perfectionist
- Diet culture: dieting involves food restriction. This food restriction and the distinction between allowed and forbidden foods seems to increase the risk of developing binge eating disorder
- Media pressure: being exposed to such pressure focused on body image, weight and dieting significantly increases the risk.
Binge eating disorder and anorexia
Binge eating disorder is closely related to other eating disorders. For example, binge eating disorder can be confused with bulimia nervosa because in both cases compulsive eating patterns in short periods of time, feelings of loss of control and feelings of guilt are observed. However, in case of binge eating disorder, there are no purging behaviours afterwards, i.e. there is no use of laxatives, no self-induced vomiting and no behaviour to compensate food intake (e.g. intense physical exercise after eating, etc.).
Regarding anorexia, food restriction associated with concerns about body weight is the reference point in contrast to binge eating disorder. People with anorexia drastically restrict their food intake in order to reduce their body weight and also show deep fear of gaining weight, even when their weight is below what is considered healthy, and may severely compromise both their nutritional status and health.
Thus, there is a distortion of their self-image or their own weight. In addition, people with purging-type anorexia engage in compensatory behaviours using laxatives and diuretics, or self-induced vomiting despite having ingested minimal amounts of food. However, they may also have episodes of binge eating that are always followed by purging behaviours.
In any case, the boundary among eating disorders is blurred and it is necessary to make the appropriate diagnosis in order to carry out the most effective intervention.
How to overcome it?
Binge eating disorder undoubtedly requires a multidisciplinary approach taking into account both the symptoms and risk factors that have been mentioned above. Intervention strategies under the premises of general health psychology should be aimed not only at reducing binge eating episodes but also at detecting the main factors that trigger these episodes (negative thoughts or emotions), improving our body image perception and establishing a conscious relationship with food based on the healthy eating habits development.
On a psychological level, cognitive behavioural therapy, both individually and in group sessions, will help the person suffering from the disorder to identify the negative thoughts and emotions that lead to the binge eating episode, as well as providing tools to cope with stress and negative emotions, and to improve their self-esteem and their body image perception.
Mindfulness-based therapy can have a complementary effect by promoting emotion regulation and developing awareness of the hunger-satiety trade-off. In addition, the concept of “Mindful Eating” has recently been developed, where the attentional focus is on the experience of eating without judgement and on the bodily sensations, thoughts and emotions that occur in the present moment, thus implementing a more conscious relationship with food.
On the other hand, nutritional intervention by the appropriate professional is required to help the person with the disorder to develop healthy eating habits and to banish the concept of dieting. Indeed, nutritional education allows routines and habits changing related to food, going deeper into the nutrients that the body needs and thus favouring the acquisition of healthy eating habits.
If, after reading this article, you find yourself reflected or you find yourself with emotions that are difficult to manage, please do not hesitate to get in touch with us.
Bibliographic references
Giel, K. E., Bulik, C. M., Fernandez-Aranda, F., Hay, P., Keski-Rahkonen, A., Schag, K., Schmidt, U., & Zipfel, S. (2022). Binge eating disorder. Nature reviews. Disease primers, 8(1), 16. https://doi.org/10.1038/s41572-022-00344-y
Loria Kohen, V., Campos del Portillo, R., Valero Pérez, M., Mories Álvarez, M.T., Castro Alija, M.J., Matía-Martín, M.P., & Gómez Candela, C.. (2021). Protocolo de educación nutricional en el tratamiento de los trastornos de la conducta alimentaria en el ámbito clínico y asistencial. Nutrición Hospitalaria, 38(4), 857-870.https://dx.doi.org/10.20960/nh.03617
Omiwole, M., Richardson, C., Huniewicz, P., Dettmer, E., & Paslakis, G. (2019). Review of Mindfulness-Related Interventions to Modify Eating Behaviors in Adolescents. Nutrients, 11(12), 2917. https://doi.org/10.3390/nu11122917
Laura N. Roza Amengual
Psychologist B-02389